More Information
Submitted: February 02, 2026 | Accepted: February 06, 2026 | Published: February 09, 2026
Citation: Mamad A, Elafari MA, Bibat MA, Moncef M, Slaoui A, Karmouni T, et al. Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case Report. J Clin Med Exp Images. 2026; 10(1): 003-005. Available from:
https://dx.doi.org/10.29328/journal.jcmei.1001039.
DOI: 10.29328/journal.jcmei.1001039
Copyright license: © 2026 Mamad A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Iatrogenic ureteral injury; Ureteral stenosis; Hydronephrosis; Pyelonephritis
Obstructive Pyelonephritis Due to Postoperative Ureteral Stricture: A Case Report
Ayoub Mamad*, Mohammed Amine Elafari, Mohammed Amine Bibat, Midaoui Moncef, Amine Slaoui, Tarik Karmouni, Abdelatif Koutani and Khalid Elkhader
Urology B Department, IBN Sina Hospital, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
*Corresponding author: Ayoub Mamad, Urology B Department, Ibn Sina Hospital, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco, Email: [email protected]
Iatrogenic ureteral injury is an uncommon but potentially severe complication of abdominopelvic surgery. When not identified intraoperatively, it may present days to weeks later with flank pain, fever, urinary tract infection, and imaging evidence of obstruction. Early recognition and timely urinary diversion are essential to prevent sepsis and preserve renal function.
A 65-year-old patient underwent elective resection of an abdominal mass; pathology confirmed schwannoma. On postoperative day 15, the patient developed left flank pain and fever. Laboratory tests showed leukocytosis (WBC 15,000/mm³) and elevated C-reactive protein (150 mg/L); urine culture grew Escherichia coli. Contrast-enhanced CT demonstrated left hydronephrosis without stones, suggesting postoperative ureteral obstruction. Retrograde double-J stenting was attempted but failed. Urgent percutaneous nephrostomy achieved decompression with clinical improvement under targeted antibiotics. Definitive exploration revealed a 1 cm stricture of the lumbar ureter, managed by segmental resection and tension-free spatulated termino-terminal ureteroureterostomy over an internal stent. Postoperative recovery was uncomplicated; the stent was removed after 3 weeks. Follow-up ultrasound showed no persistent pelvicalyceal dilatation.
Delayed ureteral obstruction should be suspected in postoperative patients presenting with flank pain, fever, and hydronephrosis. When retrograde stenting fails in the setting of infection, percutaneous nephrostomy provides rapid decompression and source control, allowing delayed definitive reconstruction. For short-segment proximal or mid-ureter strictures, ureteroureterostomy remains a reliable option when performed according to reconstructive principles.
Iatrogenic ureteral injury can occur during abdominopelvic surgery due to the ureter’s proximity to major vascular and visceral structures, with mechanisms including ligation/entrapment, transection, devascularization, crush, or thermal damage [1,2]. When unrecognized intraoperatively, it often presents later with nonspecific symptoms such as flank pain, fever, sepsis, urinoma, or imaging evidence of obstruction [1,3]. CT urography with an excretory phase is recommended to evaluate obstruction and/or urine leak [1]. In delayed cases, initial management prioritizes urinary diversion (stent or nephrostomy) and infection control, followed by definitive repair when required [1,4,5]. We report a delayed left ureteral stenosis after abdominal mass surgery managed with staged drainage and termino-terminal reconstruction [1,6].
A 65-year-old patient underwent elective surgical excision of an abdominal mass. The procedure was performed via an open approach. Intraoperatively, the tumor was located in proximity to the ureter and required careful dissection for complete removal. No ureteral injury was identified during surgery. Final histopathology confirmed schwannoma. The immediate postoperative course was initially unremarkable.
On postoperative day 15, the patient presented with left flank pain and fever, clinically consistent with acute pyelonephritis. Laboratory evaluation revealed leukocytosis (WBC 15,000/mm³) and elevated C-reactive protein (150 mg/L). Urine culture (ECBU) grew Escherichia coli, and appropriate antibiotic therapy was initiated.
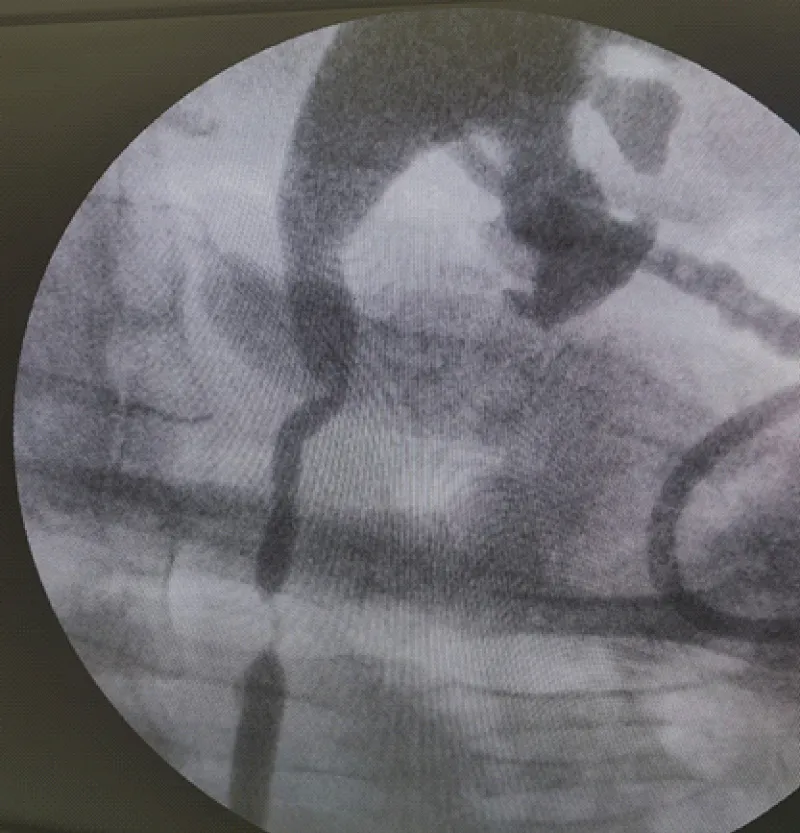
Contrast-enhanced CT demonstrated left-sided hydronephrosis/upper urinary tract dilatation without evidence of urolithiasis, raising suspicion for postoperative ureteral obstruction. Retrograde ureteral catheterization with attempted double-J stent placement was unsuccessful because the obstructed segment could not be traversed (Figure 1).
Figure 1: Retrograde attempt at ureteral stenting demonstrating inability to traverse the obstructed left ureteral segment.
Given concomitant infection and obstruction, urgent percutaneous nephrostomy was performed, resulting in immediate decompression and clinical improvement. The patient completed antibiotic therapy tailored to the culture results and remained clinically stable.
After resolution of sepsis and optimization for surgery, definitive exploration identified a short-segment stricture of the lumbar ureter measuring approximately 1cm. The stenotic segment was resected, and a tension-free spatulated termino-terminal ureteroureterostomy was performed over an internal ureteral stent, with external drainage according to institutional protocol.
Postoperative recovery was uneventful. The ureteral stent was removed 3 weeks later. Follow-up ultrasound showed resolution of hydronephrosis, with no dilatation of the pyelocaliceal system.
This case illustrates a delayed presentation of iatrogenic ureteral obstruction following abdominopelvic surgery, revealed by obstructive acute pyelonephritis. Delayed recognition is frequent because early postoperative manifestations are often non-specific and may be misattributed to postoperative pain, ileus, or unrelated infection. Recent data confirm that delayed diagnosis is associated with increased morbidity, including more readmissions, longer hospital stay, and a higher number of procedures compared with intraoperative recognition [3]. This time course is consistent with international guideline observations that most iatrogenic urinary tract injuries are detected postoperatively, typically around the second postoperative week [2].
When a postoperative ureteral injury or obstruction is suspected, prompt imaging is essential. The EAU Guidelines on Urological Trauma emphasize that contrast extravasation may be the hallmark sign when present, but that hydronephrosis or subtle ureteral dilatation can be the only radiologic finding; when CT is equivocal, retrograde or antegrade urography provides the best confirmation [1]. In our patient, CT demonstrated left hydronephrosis without calculi, supporting a postoperative obstructive mechanism rather than lithiasis.
In delayed presentations complicated by infection, management priorities are urgent source control and renal preservation. Current guidelines and expert recommendations support attempting retrograde ureteral stenting when feasible; however, failure is expected when the obstructed segment cannot be traversed. In this context, particularly with pyelonephritis or sepsis, percutaneous nephrostomy provides rapid and reliable decompression. The American Urological Association (AUA) Urotrauma guideline (2020 amendment) explicitly supports nephrostomy drainage when ureteral stenting is not possible or fails to provide adequate urinary diversion [4]. Contemporary interventional radiology series also report favorable outcomes with anterograde/percutaneous multi-step strategies, with high clinical success and preserved renal function, highlighting the value of early drainage and endoluminal salvage when possible [5]. In selected complex cases, combined antegrade–retrograde “rendezvous” approaches may facilitate stent placement and restoration of ureteral continuity, as reflected in the European Association of Urology (EAU) guidance that stenting can be performed retrogradely, antegradely, or with combined techniques [1].
Definitive repair is determined by lesion location and length, tissue viability, and the feasibility of a tension-free reconstruction. For short-segment proximal or mid-ureteral strictures, segmental resection with spatulated tension-free ureteroureterostomy over a stent remains a standard reconstructive option, provided well-vascularized ends can be approximated [1]. Recent reconstructive literature and expert-derived algorithms emphasize core principles- healthy tissue, wide spatulation, tension-free anastomosis, and adequate drainage- and place ureteroureterostomy among preferred strategies for short strictures in the proximal/mid ureter, while longer defects may require ureteroneocystostomy (± psoas hitch/Boari flap), substitution techniques, or other complex reconstructions [6]. In our case, a staged approach-urgent decompression and antibiotics followed by delayed reconstruction after resolution of infection-aligned with these principles and resulted in a favorable outcome.
In postoperative patients presenting with flank pain, fever, and hydronephrosis, iatrogenic ureteral obstruction should be actively considered. CT with an excretory/urographic phase, followed by retrograde or antegrade urography when needed, is central for diagnosis [1]. In the presence of infection and obstruction, urgent urinary diversion is mandatory; if retrograde stenting fails, percutaneous nephrostomy provides effective decompression and stabilization [4,5]. For short-segment lumbar/proximal or mid-ureter strictures, termino-terminal ureteroureterostomy is a reliable definitive option when reconstructive principles are respected [1,6].
- European Association of Urology. EAU guidelines on urological trauma. Arnhem; 2025. Available from: https://uroweb.org/guidelines/urological-trauma/summary-of-changes/2025
- de'Angelis N, Schena CA, Marchegiani F, Reitano E, De Simone B, Wong GYM, et al. 2023 WSES guidelines for the prevention, detection, and management of iatrogenic urinary tract injuries (IUTIs) during emergency digestive surgery. World J Emerg Surg. 2023;18(1):45. Available from: https://doi.org/10.1186/s13017-023-00513-8
- Maheswaran R, Beisland C, Bergesen AK, Almås B. A delayed diagnosis of iatrogenic ureteral injury results in increased morbidity. Sci Rep. 2024;14(1):13771. Available from: https://www.nature.com/articles/s41598-024-63847-6
- Morey AF, Broghammer JA, Hollowell CMP, McKibben MJ, Souter L. Urotrauma guideline 2020: AUA guideline. J Urol. 2021;205(1):30-35. Available from: https://doi.org/10.1097/JU.0000000000001408
- Barabino E, Nivolli A, Tosques M, Ivaldi D. Percutaneous management of iatrogenic ureteral injuries using a multistep approach: Clinical, functional and long-term outcomes. Abdom Radiol. 2025:1-10. Available from: https://doi.org/10.1007/s00261-025-04902-2?urlappend=%3Futm_source%3Dresearchgate.net%26utm_medium%3Darticle
- Bourillon A, Peyronnet B, McGuire BB, Pinar U, Lee Z, Nair R, Stifelman M, et al. Ureteral stricture: Current treatment algorithm and key surgical principles in the robotic upper urinary tract reconstruction era. World J Urol. 2026;44(1):102. Available from: https://link.springer.com/article/10.1007/s00345-025-06181-4