Abstract
Observational Study
Establishment of a Best Practice Recommendation (BPR) for Abdominal Aortic Aneurysms in a Large Multi-State Radiology Practice: Adoption and Impact
Andrew K Hillman, Phil Ramis, Patrick Nielsen and Eric M Rohren*
Published: 26 August, 2024 | Volume 8 - Issue 1 | Pages: 007-012
Purpose of the study: To evaluate the performance of Best Practice Recommendation (BPR) compliance in reporting abdominal aortic aneurysm findings on imaging, comparing the results before and after its deployment.
Methods: Best Practice Recommendations for AAA were deployed in 2020 at a large radiology practice site. Reports between January 2018 through October 2022 were reviewed, representing studies read prior to and subsequent to the implementation of the reporting standards. Cases of abdominal aortic aneurysms ≥ 2.6 cm were counted by year. Adherence to the BPR for each year was calculated as [total number of confirmed cases of ≥ 2.6 cm AAAs with compliant reports] * 100 / [the total number of confirmed ≥ 2.6 cm AAAs]. A secondary analysis was performed to determine whether there was a statistically significant difference in the proportion of BPR-compliant reports for AAA cases before (from 2018 to 2019) and after (from 2020 to 2022) BPR deployment using a chi-square test.
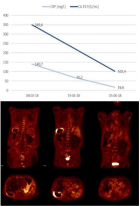
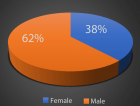
Results: From January 2018 to December 2022, there were 8,693 reports referencing AAA. After excluding cases of suspected AAA (N = 2,131), confirmed AAAs with indeterminate sizes (N = 103), and confirmed AAAs with sizes < 2.6 cm (N = 85), the number of AAA cases ≥ 2.6 cm in size was 6,374. Concordance with the BPR standards for the remaining cases with sizes ≥ 2.6 cm were 1.6% and 4.1% in 2018 and 2019, respectively. Post-implementation of BPRs, there was a substantial improvement in guideline adherence to 32.1%, 84.3%, and 83.6% in 2020, 2021, and 2022, respectively.
In general, the proportion of BPR-compliant reports of AAA cases in the pre-deployment (3.6%) period statistically differs (p - value < 0.0001) from those in the post-deployment period (73.9%)
Conclusion: Adherence to reporting standards increased after the BPR deployment in 2020. The inclusion of management recommendations in the radiology report when AAA is identified is a simple and cost-effective way of improving outcomes for patients with AAAs through appropriate follow-up treatment.
Read Full Article HTML DOI: 10.29328/journal.jcmei.1001032 Cite this Article Read Full Article PDF
Keywords:
Abdominal aortic aneurysms; Best practice recommendations; Quality Improvement
References
- Shaw PM, Loree J, Gibbons RC. Abdominal Aortic Aneurysm. [Updated 2023 Mar 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470237/
- Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: The impact of size, gender, and expansion rate. Journal of Vascular Surgery. 2003 Feb;37(2):280-4. https://doi.org/10.1067/mva.2003.119
- D'Souza D, Weerakkody Y, Alhusseiny K. Abdominal aortic aneurysm [internet]. Radiopaedia.org.[cited 2023 March 28]. Available from: https://radiopaedia.org/articles/abdominal-aortic-aneurysm?lang=us
- Ahmed S, Mitsky J, Rawal U, Sheth S, Bronner J. Asymptomatic Abdominal Aortic Aneurysm: Standardizing Reporting Recommendations at a Large Multistate Radiology Practice. Journal of the American College of Radiology. 2021 Sep;18(9):1317-23. https://doi.org/10.1016/j.jacr.2021.04.009
- Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL. Managing Incidental Findings on Abdominal and Pelvic CT and MRI, Part 2: White Paper of the ACR Incidental Findings Committee II on Vascular Findings. Journal of the American College of Radiology. 2013 Oct;10(10):789-94. https://doi.org/10.1016/j.jacr.2013.05.021
- Chung J. Epidemiology, risk factors, pathogenesis, and natural history of abdominal aortic aneurysm [internet]. UptoDate.com. [cited 2023 March 28]. Available from: https://www.uptodate.com/contents/epidemiology-risk-factors-pathogenesis-and-natural-history-of-abdominal-aortic-aneurysm
- Dent TL. Multiple Arteriosclerotic Arterial Aneurysms. Archives of Surgery, 1972 Aug 1;105(2):338 https://doi.org/10.1001/archsurg.1972.04180080184031
- Rouchaud A, Brandt M, Rydberg A, Kadirvel R, Flemming K, Kallmes D, Brinjikji W. Prevalence of Intracranial Aneurysms in Patients with Aortic Aneurysms. AJNR American Journal of Neuroradiology. 2016 Sep;37(9):1664-8. https://doi.org/10.3174/ajnr.a4827
- Aggarwal S, Qamar A, Sharma V, Sharma A. Abdominal aortic aneurysm: A comprehensive review. Experimental & Clinical Cardiology, 2011;16(1):11-5. https://pubmed.ncbi.nlm.nih.gov/21523201/
- Brox AC, Filion KB, Zhang X, Pilote L, Obrand D, Haider S, Azoulay A, Eisenberg MJ. In-Hospital Cost of Abdominal Aortic Aneurysm Repair in Canada and the United States. Archives of Internal Medicine, 2003 Nov 10;163(20):2500. https://doi.org/10.1001/archinte.163.20.2500
- Peek KN, Khashram M, Wells JE, Roake JA. The costs of elective and emergency abdominal aortic aneurysm repair: a comparative single centre study. New Zealand Medical Journal, 2016 Apr 22;129(1433):51-61. https://pubmed.ncbi.nlm.nih.gov/27349161/
- Abdominal aortic aneurysm: Screening. (2019, December 10). Uspreventiveservicestaskforce.org; US Preventive Services Taskforce. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/abdominal-aortic-aneurysm-screening
- Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. Journal of Vascular Surgery. 2018 Jan;67(1):2-77.e2. https://doi.org/10.1016/j.jvs.2017.10.044
- Karthaus EG, Tong TML, Vahl A, Hamming JF. Saccular Abdominal Aortic Aneurysms. Annals of Surgery. 2019 Nov;270(5):852-8. https://doi.org/10.1097/sla.0000000000003529
Figures:
Similar Articles
-
Establishment of a Best Practice Recommendation (BPR) for Abdominal Aortic Aneurysms in a Large Multi-State Radiology Practice: Adoption and ImpactAndrew K Hillman, Phil Ramis, Patrick Nielsen, Eric M Rohren*. Establishment of a Best Practice Recommendation (BPR) for Abdominal Aortic Aneurysms in a Large Multi-State Radiology Practice: Adoption and Impact. . 2024 doi: 10.29328/journal.jcmei.1001032; 8: 007-012
Recently Viewed
-
Hypoglycemia by Ginseng in type 2 Diabetic Patient: Case ReportAngelo Michele Carella*,Teresa Marinelli,Armando Melfitano,Michele Di Pumpo,Matteo Conte,Angelo Benvenuto. Hypoglycemia by Ginseng in type 2 Diabetic Patient: Case Report . New Insights Obes Gene Beyond. 2017: doi: 10.29328/journal.hodms.1001001; 1: 001-006
-
Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary SurveyFatimah M Kaabi,Layth Mula-Hussain*,Shakir Al-Shakir,Sultan Alsaiari,Leonidas Chelis,Renda AlHabib,Sara Owaidah,Renad Subaie,Marwah M Abdulkader,Ibrahim Alotain. Unveiling Disparities in WHO Grade II Glioma Care among Physicians in Middle East and North African (MENA) Countries: A Multidisciplinary Survey. Arch Cancer Sci Ther. 2026: doi: 10.29328/journal.acst.1001048; 10: 001-005
-
Analysis and Control of a Glucose-insulin Dynamic ModelLakshmi N Sridhar*. Analysis and Control of a Glucose-insulin Dynamic Model. Ann Clin Endocrinol Metabol. 2026: doi: 10.29328/journal.acem.1001033; 10: 010-016
-
NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and MuscleRizwan Uppal,Umar Saeed*,Muhammad Rehan Uppal. NAD⁺ Biology in Ageing and Chronic Disease: Mechanisms and Evidence across Skin, Fertility, Osteoarthritis, Hearing and Vision Loss, Gut Health, Cardiovascular–Hepatic Metabolism, Neurological Disorders, and Muscle. Ann Clin Endocrinol Metabol. 2026: doi: 10.29328/journal.acem.1001032; 10: 001-009
-
Nasal cytology in patients with previous SARS-CoV-2 infection: occurrence of atypical lymphocytesArturo Armone Caruso*, Anna Miglietta, Giovanni De Rossi, Liliana Nappi, Veronica Viola, Stefano De Rossi, Salvatore Del Prete, Clara Imperatore, Sabato Leo, Daniele Naviglio, Monica Gallo, Daniela Marasco, Lucia Grumetto. Nasal cytology in patients with previous SARS-CoV-2 infection: occurrence of atypical lymphocytes. Adv Treat ENT Disord. 2023: doi: 10.29328/journal.ated.1001014; 7: 001-006
Most Viewed
-
Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trialSathit Niramitmahapanya*,Preeyapat Chattieng,Tiersidh Nasomphan,Korbtham Sathirakul. Effects of dietary supplementation on progression to type 2 diabetes in subjects with prediabetes: a single center randomized double-blind placebo-controlled trial. Ann Clin Endocrinol Metabol. 2023 doi: 10.29328/journal.acem.1001026; 7: 00-007
-
Physical Performance in the Overweight/Obesity Children Evaluation and RehabilitationCristina Popescu, Mircea-Sebastian Șerbănescu, Gigi Calin*, Magdalena Rodica Trăistaru. Physical Performance in the Overweight/Obesity Children Evaluation and Rehabilitation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001030; 8: 004-012
-
Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging PresentationKarthik Baburaj*, Priya Thottiyil Nair, Abeed Hussain, Vimal MV. Hypercalcaemic Crisis Associated with Hyperthyroidism: A Rare and Challenging Presentation. Ann Clin Endocrinol Metabol. 2024 doi: 10.29328/journal.acem.1001029; 8: 001-003
-
Exceptional cancer responders: A zone-to-goDaniel Gandia,Cecilia Suárez*. Exceptional cancer responders: A zone-to-go. Arch Cancer Sci Ther. 2023 doi: 10.29328/journal.acst.1001033; 7: 001-002
-
The benefits of biochemical bone markersSek Aksaranugraha*. The benefits of biochemical bone markers. Int J Bone Marrow Res. 2020 doi: 10.29328/journal.ijbmr.1001013; 3: 027-031

If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."